Case Study: Radiation Retinopathy JPD
78 yo woman with past medical history of NAAION OD presents with flashes and floaters OS. Her visual acuity is 20/70 OD and 20/30 OS. Her intraocular pressures were 14 OD and 16 OS. Her anterior segment exam was normal. On funduscopic exam OS she was found to have diffuse disc pallor. On funduscopic OD she was found to have elevated choroidal lesion with orange pigment in the superonasal midperiphery.

She underwent Iodine125 plaque radiation therapy, with placement of a 14mm radioactive plaque for 91 hours for a total delivered dose of 84.5 Gy.
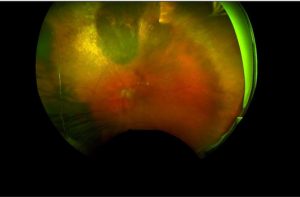
The tumor regressed postoperatively, and her metastatic workup showed no evidence of metastatic disease. There was no recurrence of the tumor.
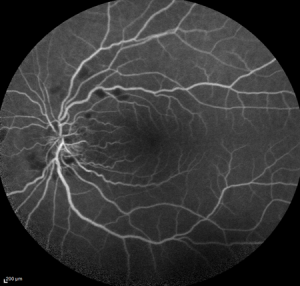
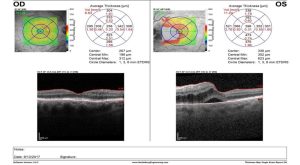
However, her vision OS declined from 20/30 preoperatively to 20/200 postoperatively. Her clinical examination showed cotton-wool infarcts, intraretinal hemorrhages, and blunting of foveal reflex .
And her OCT revealed retinal thickening OS.
Radiation Retinopathy occurs in approximately half of patients who receive plaque brachytherapy (42-53%).
It presents clinically as intraretinal hemorrhage, microaneurysms, cotton-wool spots, vascular telangiectasia, hard exudates, and macular edema, and can involve retinal neovascularization, vitreous hemorrhage, and exudative retinal detachment.
There is yet no effective means of preventing radiation retinopathy. Silicone oil and perfluorocarbon liquids have been used with limited success.
Anti-VEGF therapy has become the standard of care in management of radiation retinopathy and is helpful in controlling retinal thickening.
Plaque brachytherapy is a very effective tool in the management of ocular melanoma, controlling growth and spread of the tumor in~90% of cases. Anti-VEGF therapy can provide some vascular leakage and macular edema associated with radiation retinopathy.
